Part 1: We work hard for the money (and by money, I mean $29.61)
By Katie Stoll, MS, CGC
In this series, we will review challenges with reimbursement for genetic counseling services. The current system undervalues genetic counseling, leading to a strain on clinics and hospitals, overutilization of genetic tests, burnout for genetic counselors, and suboptimal patient care. We will consider how we got here and how we might move forward in a more sustainable way.
In 1992, the Washington State’s Medicaid program became the first to reimburse genetic counseling services. Now, more than 30 years later, genetics is becoming an integral component of many areas of medicine. Despite this, genetic counseling services are still not reimbursed consistently. Medicare does not recognize genetic counselors as qualified providers for reimbursement of services, most other Medicaid programs do not reimburse, and private insurers provide mixed coverage and reimbursement.
While I feel fortunate to live in a state that recognizes genetic counselors, I find the overall landscape of reimbursement for genetic services to be deeply problematic. This year, the Washington State Health Care Authority has set the fee for genetic counseling services at $29.61 for each genetic counseling unit, which is recognized by the CPT code 96040. This is a time-based code and can be stacked up to 3 times, such that a genetic counseling consultation of 16-45 minutes is equivalent to 1 unit, 46-75 minutes is 2 units, and 76 minutes and beyond is 3 units. This means that even for the most complex and lengthy of genetic counseling encounters, the most that genetic counseling would be reimbursed by Washington Medicaid is $88.83. For comparison, the “low complexity” CPT code for occupational therapists (97165) reimburses $59.92 for 30 minutes. This is more than double the reimbursement for genetic counselors for face-to-face time.
This rate is set based on a complicated formula that takes into account the fee set by Centers for Medicare and Medicaid Services (CMS). Surprisingly, CMS does assign a value to the genetic counseling code, even though they note that Medicare will not reimburse for it.
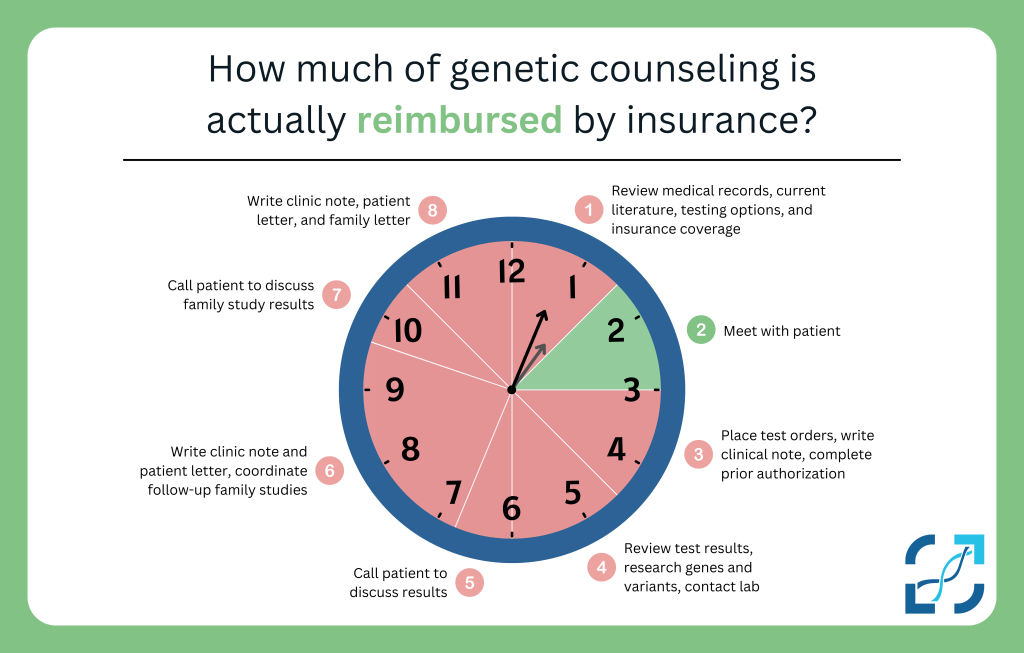
It is also important to note that this fee is only paid for the actual face-to-face time that a genetic counselor spends with a patient. There is no reimbursement for all of the other work we do to support each patient. For any given patient we may spend hours collecting and reviewing medical records, researching relevant medical conditions and specific genes and variants, following-up and coordinating with family members, communicating with insurance companies for pre-authorizations and denial appeals, coordinating test sample collection, writing clinic notes and family letters, and more.
Below I will illustrate a case to highlight the work of a genetic counselor and the reimbursement for this work:
A pregnant patient is referred for genetic counseling because an 18-week ultrasound revealed multiple findings that were concerning for serious health problems. There appears to be a heart defect, the kidneys and brain are not developing normally, and the baby is measuring as much smaller than would be expected for the gestational age.
20 minutes – The genetic counselor reviews the medical records in preparation for meeting with the patient, reviews testing options and the patient’s insurance, and relevant literature
60 minutes* – The genetic counselor meets with the patient face-to-face and provides psychosocial support as well as information about what the ultrasound findings could mean, possible diagnoses, and the chance of recurrence in future pregnancies. The pregnancy history and family health history are reviewed in detail and the risks, benefits, and limitations of genetic testing options are discussed.
During the genetic counseling visit, the couple share their commitment to continuing the pregnancy regardless of any prenatal diagnosis. They would like to better understand the potential cause of the findings so they can prepare for what to expect for the pregnancy and following birth. They elect to proceed with diagnostic testing, which involves an amniocentesis procedure and a karyotype and chromosomal microarray test.
20 minutes – The genetic counselor places all orders in the health electronic record and lab portals, ensuring that all details are included to inform laboratory interpretation of any identified genetic variants.
60 minutes – The genetic counselor writes a detailed consult note back to the referring obstetrician’s office, outlining the discussion, risk assessment, and plan for next steps. This detailed consult note will also be required as supporting documentation to obtain authorization from insurance for the ordered genetic testing.
The karyotype returns showing a fetal diagnosis of trisomy 13. The chromosomal microarray also finds a small duplication of genetic material on the X chromosome. Conditions on the X-chromosome can be carried silently by the parent and passed on to children who will be affected, especially if they are assigned male at birth. It is not known whether or not the specific duplication found on the test has any clinical significance. In other words, carrying this variation may not cause any serious health concerns. However, because it has not been reported in the medical literature previously, testing of family members is recommended to help clarify whether this variant is associated with potential health risks for future pregnancies.
45 minutes – The genetic counselor researches this duplication and the genes in this region and has a discussion with the lab staff to better understand the potential significance of these results before calling the patient.
30 minutes – The genetic counselor calls the patient to review the results in detail. She is scheduled to return for a follow-up ultrasound and genetic counseling appointment later that week.
30 minutes – The genetic counselor writes a detailed note to the referring obstetrician and to the patient outlining the test results and what is known about their clinical significance.
10 minutes* – The patient returns for ultrasound and learns that there has been a demise – there is no heartbeat. It is not uncommon for pregnancies with trisomy 13 to end in stillbirth. The genetic counselor meets with the couple again briefly to provide support, however, given the shock of this news they would like to defer further discussion about the test results to a later date.
Follow-up studies on a sample of the patient’s blood reveal that she also carries the X chromosome duplication that was seen in the fetus. Fetal autopsy shows numerous birth defects that are consistent with a diagnosis of trisomy 13. Trisomy 13 is not inherited and the recurrence risk is up to 1% or based on parental age, whichever is higher. It is still unclear if the X chromosome duplication has any significance for future pregnancies.
30 minutes – The genetic counselor calls the patient to review the genetic test results and discuss next steps. The genetic counselor explains that by testing the patient’s father and/or brother, who report no related-symptoms, they may gain more information. If either or both carry this same duplication, the lab has indicated that the duplication would be reclassified as a benign polymorphism – in other words, a duplication that is of no concern for health risks for the patient’s future children. The patient and her partner decide to pursue family studies of the duplication for more information.
20 minutes – The genetic counselor talks with the lab about coordinating obtaining samples from the family members.
30 minutes – The genetic counselor coordinates the blood sample collection for the family members with their primary care providers.
The results return for the patient’s father and brother. They both carry the same duplication as the patient, and thus, it is highly unlikely that this duplication would present health risks for the couple’s future children. The couple are appreciative of this information and indicate their plans to try for another pregnancy sometime in the next few months.
30 minutes – The genetic counselor calls the patient to review these results and answer questions.
20 minutes – The genetic counselor writes a brief note back to the referring provider to summarize the findings.
*Only face-to-face time spent with the patient is reimbursable by insurance and the length of time must be 16 or more minutes in order to submit a claim.
This case illustrates a realistic summary of all that is involved in providing genetic counseling to a patient with complex concerns. Similar examples could be outlined for genetic counseling in other specialties, including but not limited to, pediatrics, neurogenetics, cardiogenetics, and hereditary cancer. As genetic counselors, we often work through medically complicated and emotionally difficult situations with families that may involve weeks or even months of research, follow-up testing, and additional non face-to-face counseling. Genetic counseling services are crucial to the families going through these difficult circumstances, and no genetic counselor I know would rush through these encounters at the expense of providing the family all of the support they need. I also believe that healthcare systems want to provide these essential services to patients, not only because it is important care, but also to reduce their own liability. Genetic counselors are uniquely qualified to do this work.
In this case, I conservatively estimate 6.75 hours of actual genetic counselor time, however, only one hour of that is reimbursable time. If the patient’s insurance is Washington State Medicaid, then this work would be reimbursed with $59.22 equating to less than $9/hour if we consider all of the time invested.
You may be thinking that private insurance would surely reimburse much more for genetic counseling, but while the fees set by commercial insurances for genetic counseling may be multiples of the Medicaid rate, it still does not come close to sustainably compensating the work of genetic counselors. At GSF we have seen commercial insurance companies that we are contracted with refuse to reimburse for indications that should be covered by their own published policies. We have seen commercial payers reimburse us, and then send us a bill, many months later stating that per their review, they do not think they should have actually paid for the service and demanding that we pay them back.
At GSF, it is our mission to increase access to genetic counseling services and to see that genetic counseling is sustainable as an independent practice, not bundled into the fees charged by labs for genetic testing. Consistent with this mission, we will continue to advocate for fair reimbursement, and seek reimbursement from insurance payers for our services. It is a painful process though, and we understand why many hospitals and clinics do not bother billing insurance for the services provided by genetic counselors. The difficult reality is that in most cases, the resources we invest in just attempting to collect reimbursement far exceed what we are reimbursed and do not come close to covering our time.
Despite the insufficient reimbursement by insurance for genetic counseling, the salary for genetic counselors is shooting upwards. According to the National Society of Genetic Counselors Professional Status Survey, the average salary for a genetic counselor in 2024 was over $104K. This is compared to about $74K in 2014 and $53K in 2002. Although the salaries of genetic counselors have nearly doubled in the last 20 years, reimbursement by Medicaid and health insurance has remained stagnant, threatening the financial sustainability of this critical profession.
If you are a patient who is facing insurance barriers to receiving the genetic counseling you need, we are with you. If you are a genetic counselor out there who is exhausted by constantly having to justify your value and your time, we hear you. If you are a hospital administrator who is having a difficult time penciling out how to pay for a genetic counselor on staff or contracting with an organization like Genetic Support Foundation to provide services, we understand. Having a genetic counselor as part of a healthcare team is becoming increasingly necessary to provide comprehensive and complete healthcare, but the difficult reality is that as it stands now, genetic counseling services often do not generate much, if any billable revenue. How did we get to the point where the reimbursable rate for genetic counseling is so, so much less than the salaries paid to genetic counselors? How do we see this evolving over the next 20 years?
We will consider these questions in future posts. Stay tuned for the next entries in this series to learn more.